Quickly find the answers you may need as you enjoy quality wellness benefits with our BeWell Welcome Guide.
EMI Health ID Card
You will receive your Member ID Card in the mail after enrollment. The card lists the subscriber's name only, but can be used by all plan members.
Your EMI Health ID card is more than just proof of insurance–it's a quick reference for you and your providers. It lists your plan types, provider networks, and essential contact information.
Each card is personalized based on your coverage. If your card includes medical, dental, and vision plans, each section will appear in its own tab. If you only have one type of coverage (such as dental), all your plan details may appear on one side of the card.
How to Search for a Provider
As a member of EMI Health, you can take advantage of a large choice of in- network providers locally and nationally. To find an in- network provider, follow these steps.
- Go to emihealth.com and click on + FIND A PROVIDER along the upper part of the home page, or use the green button below.
- Choose Search as a Guest*
- Click on either the MEDICAL, DENTAL, or VISION tab, Choose your NETWORK NAME from the drop down menu, Choose your STATE, and click SEARCH.
Scroll down to see a list of participating providers along with their contact information. If you'd prefer to search for a specific provider, enter the PROVIDER NAME in the field and click the SEARCH button.
*If you are already a member, Click Search as a Member, you will be directed to register or login to your My EMI Health Account. From your member dashboard, you can select +Find a Provider and your default networks will be auto-populated. It's a quick and easy way to search for all your in-network providers.
Understanding Claims
Carrier Vs. Network
EMI Health is currently your insurance carrier. We pay your claims, manage your plan, and coordinate your benefits. It's important to remember that we are the main point of contact for eligibility, pre-authorizations, and all other benefit questions. In addition to providing insurance services, we lease provider networks to give you substantial discounts on your medical services and give you the convenience of having in-network provider options wherever you are in the country.
Some of the provider networks we lease are Aetna, Blue Cross Blue Shield, Cigna, or First Health. It will vary depending on what state you are in and your plan. Please check your ID card for your in- state network information and note it may be a different than the out-of- state network.
Your ID card also includes a section for your provider indicating how and where to submit claims. It's important that your claims get submitted to the correct network and that your provider uses the correct claim address (found on your ID card) to ensure you're getting that special rate and the best savings.
EOB's (Explanation of Benefits)
Your Explanation of Benefits (EOB) shows you the details of your insurance claim. It shows when you received the service and it explains how much of the service was paid by your insurance and how much, if any, is your responsibility. At EMI Health, your EOBs are emailed to you when they are processed. They are then stored in your My EMI Health online account. We do not send paper copies, so it is important to check your dashboard regularly to view your most recent claims and associated EOBs.
It's a simple 3- step process to find them in your member account:
- Log in to your My EMI Health account.
- In the Recent Claims section, to the right of each claim, you will see the View EOB button.
- Filter your results: You can sort your claims by type, family member, time period, or network using the drop down menus at the top. You can see more claims by clicking on Advanced Claims Search.
In less than 30 seconds, you can find the EOB you are looking for. It has never been easier to locate and view your EOBs with EMI Health.
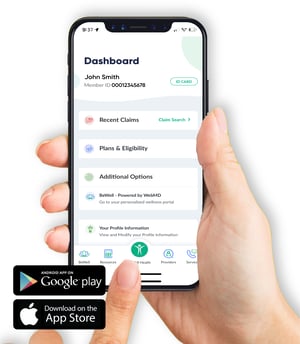
EMI Health Mobile App
Download the EMI Health mobile app to carry your benefits with you wherever you (and your phone) are headed.
Access your BeWell PortalSee your EOBs (Explanation of Benefits)Plan DocumentsSearch for a ProviderView your ID Card
Click to Download the App: For Android | For iPhone
Register your EMI Health Account
 Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Follow these steps:
- Go to https://emihealth.com/Identity/Account/Register
- Choose Member, and click Continue.
- Fill in requested information including your EMI Health Member ID number from your ID card, Click Continue.
My EMI Health Member Dashboard
Your member dashboard gives you a clear view of your benefits—all in one secure place. Use it to track claims, check coverage, download your ID card, and more.
Note: Your dashboard may look different depending on the type of benefits you have.

What You’ll Find on Your Dashboard:
✔ Member ID Card
Quickly view, download, or print your EMI Health member ID card for easy access whenever you need it.
✔ Plan Details
See which plans you're enrolled in and get quick links to plan documents like benefit summaries and coverage guides.
✔ Accumulators
Get real-time updates on how much you’ve paid toward your deductible and out-of-pocket maximum for medical and dental plans.
✔ Claims & EOBs
Check the status of your recent claims and view Explanation of Benefits (EOB) statements to understand what’s been paid and what you might owe.
✔ Provider Search
Use our upgraded search tool to find in-network doctors, dentists, and specialists—now with filters to help you narrow your results.
✔ Resource Library
Browse helpful forms, articles, and answers to common questions—all in one convenient place.
BenefitHub Discounts
Enjoy deals and discounts at your favorite stores and on your favorite brands just because you're a member of EMI Health. Discounts on over 100,000 name brands at hundreds of your favorite retailers. Find tickets to sporting events, concerts, theaters, movies and theme parks. Shop restaurants, gyms, Groupon deals and thousands of other local offers.
Start saving now:
1. Go to https://emi.benefithub.com/Welcome2. Click Create Account.3. Enter Referral Code: NV6ADR4. Enter your email address5. Click Create Account.
💡
Always show your EMI Health ID card when you check in for care. It helps avoid billing issues and makes sure your visit runs smoothly.
💡
Always show your EMI Health ID card when you check in for care. It helps avoid billing issues and makes sure your visit runs smoothly.
MEDICAL
Telehealth
Care that comes to you—anytime, anywhere with $0 cost.
As an EMI Health member, you have 24/7 access to board-certified doctors and licensed therapists through Recuro Health. Get care for everyday issues like colds, anxiety, skin conditions, or allergies—without leaving home.
No travel. No waiting rooms. No extra cost.
Lyra Mental Health Provider Network
Virtual and in- person behavioral health therapy WHEN and WHERE you need it when you use the Lyra Provider Network.
EMI Health medical members have access to Lyra Health's provider network of therapists and coaches at no additional cost. Sessions are billed as in- network outpatient, as defined under your mental health benefit.
Register/Login to Search for Lyra Provider: https://emihealth.lyrahealth.com/
Preventive Care
What is ACA preventive care—and why does it matter?
The Affordable Care Act (ACA) requires health plans to cover certain preventive care services at no cost to you—meaning no copay, no deductible, and no coinsurance when you see an in-network provider.
These services help you stay healthy and catch problems early, before they become serious.
Preventive care includes:
-
Screenings for blood pressure, cholesterol, cancer, diabetes, and more
-
Vaccines like flu shots, COVID-19, and tetanus boosters
-
Wellness visits including annual physicals and well-child checks
-
Women’s health services such as mammograms, cervical cancer screenings, and birth control
-
Pediatric care like developmental screenings and routine immunizations
👉 Just make sure your visit is billed as “preventive”—not for an existing condition or symptoms—to qualify for full coverage.
Diabetes Management
If you manage diabetes, EMI Health has you covered with testing supplies, insulin, and more. Here’s what you need to know about your benefits.
Testing Supplies
-
What’s included: Test strips, lancets, meters, and syringes
-
How it’s covered: Through your Medical or Pharmacy benefit, depending on the supplier
-
Tip: Use in-network providers for the best coverage
Insulin and Diabetes Medications
-
Insulin: Covered through your Pharmacy Benefit
-
$25 for a 30-day supply
-
$75 for a 90-day supply (if eligible through the Patient Assurance Program*)
-
-
Other covered medications: Glucagon, GLP-1s, and Type 2 oral meds
Insulin Pumps
-
Covered under: Your Medical Benefit
-
May require: Pre-authorization
-
Includes: Pumps and pump supplies
Continuous Glucose Monitors (CGMs)
-
Coverage varies: May be under Medical or Pharmacy Benefit
-
Check your plan: Some CGMs and sensors need pre-authorization
Price Transparency Tool
A tool to help you compare medical procedure costs and make informed healthcare decisions so you save money and avoid surprise charges.
What It Does
-
Shows personalized cost estimates for medical procedures before you get care.
-
Helps you compare providers by price and quality.
-
Lets you see what you’ll pay for deductibles and out‑of‑pocket cost ahead of time, so you can plan.
How to Use It
-
Log in to your EMI Health Dashboard at emihealth.com.
-
Go to Programs & Tools and click “MyMedicalShopper.”
What You Gain
-
Save time and money
-
Avoid overpaying for medical services
-
Be more secure about what medical bills might be before you agree to care
Where to go for Healthcare
Knowing where to go for care can help you get effective treatment and save money.
This information is for general guidance only and does not replace professional medical advice, diagnosis, or treatment. Coverage details may vary by plan. Always check your specific benefits, provider network, and cost-sharing responsibilities through your EMI Health member portal or by contacting Customer Service.
| Type of Need | Best Place to Go | Why It’s Smarter |
|---|---|---|
| Telehealth for minor issues | Use TeleMed | Zero cost for things like allergies, coughs, rashes, earaches, sore throat, etc. |
| Routine or non‑urgent care | Schedule with your Primary Care Provider or go to a Convenience Clinic | Less cost, more convenience |
| Urgent but non‑life‑threatening issues | Go to an Urgent Care Facility | Open longer hours, cheaper than ER for things like minor broken bones, stitches, etc. |
| Serious or life‑threatening symptoms | Go directly to the Emergency Room (ER) | For emergencies like chest pain, stroke, heavy bleeding, head/spine injury, etc. |
When to Use the ER
Go to the emergency room immediately if you’re having signs of a true medical emergency, such as:
-
Trouble breathing
-
Sudden, severe headache
-
Stroke signs
-
Seizure
-
Head or spine injury
-
Broken bone
-
Severe chest pain
-
Heavy bleeding
-
Deep wound
Tier 1/Elite Providers
Select EMI Health PPO Traditional plans include a “Elite Tier” of providers. When you choose a Tier 1 (Elite) provider, you’ll pay lower copays, $10 for general doctors, $20 for specialists—saving money while getting the same high-quality care. Your plan and network stay the same; this just gives you a new way to lower your out-of-pocket costs.
How to Use the Elite Tier
-
Find an Elite Provider
You’ll be able to see which providers are in Tier 1 (Elite) when choosing a doctor. -
Schedule your visit with an Elite Provider
Make sure you check their tier before booking. -
Enjoy savings with reduced copays
Visits with Tier 1 providers cost less than the same service with higher‑tier providers.
Reminder
-
Tier 1 copays are standard across all eligible plans. Other tiers may still have different cost levels.
-
Make sure you check your Summary of Benefits to see exactly what your copays are with Tier 2 or non‑participating providers.
Resources
View or Download Booklet: English
Garner App
Garner is a benefit that works alongside your EMI Health plan to help you find top-performing doctors—and get reimbursed for eligible medical costs. It’s a smarter, simpler way to save on care.
Set Up Your Garner Account
As soon as you’re enrolled in your EMI Health medical plan and have your Member ID number, download the Garner app and create your account.
Setting up your account early means you can start using Garner right away—to find top doctors and get money back on your medical costs.
or visit: https://app.getgarner.com/
When you register, you will choose your organization's name from the Garner app's drop-down menu. If you do not recognize your company name, contact your HR benefit's director to verify.
Learn more about Garner:
View or Download Booklet: English

- BeWell Member Guide
- Free Mental Health Coaching
- Other Mental Health Resources
- Fitness Perks
- Tobacco Cessation
- Maternity Management
- Nurse Health Coaching
- Weight Management Program
EMI Health is excited to offer a new mental health resource to our medical plan members. BeWell's Mental Health Coaching connects you with certified mental health professionals with advanced degrees, who can help you manage stress, build resilience, and support your mental health, quickly and confidentially.
EMI Health offers a variety of mental health resources to support you and your covered family members. Depending on your plan, you may have access to services like virtual or in-person therapy through Lyra, free mental health coaching with BeWell, and provider search tools to find in-network counselors, psychologists, and psychiatrists. Some members may also qualify for an Employee Assistance Program (EAP) through their employer.
Benefits may vary based on your specific plan. Be sure to check your coverage details or contact Customer Service for more information.
Join the Tobacco Cessation Program
Quitting smoking is hard, which is why EMI Health and WebMD Health Services have teamed up to make the process a little easier. This program is voluntary, completely confidential, and comes at no cost to you. Our mission is to empower members through personalized coaching to overcome high-risk habits and reclaim their long-term health.
Your path to quitting:
- Three months of 1-on-1 coaching with a BeWell health coach
- Develop personalized strategies to make quitting easier
- Explore the harmful effects of tobacco use and the benefits of quitting
- Nicotine Replacement Therapy (NRT)*
- Build positive daily habits and set small, achievable goals for long-term success
Get started today! Download the BeWell app.
- Scan the QR code below to download the Wellness at Your Side app
- Use the connection code: BeWell
- Login with your My EMI Health account credentials
Don’t have an account? Register your My EMI Health account by going to emihealth.com/account.
A free support program for pregnant members (or spouses) through their journey to having a healthy baby.
What the Program Offers
-
A Registered Nurse Specialist who works with you one‑on‑one, at no extra cost.
-
Help understanding your pregnancy stages, and what to expect.
-
Guidance on healthy diet, safe exercise, and general self‑care during pregnancy.
-
Early detection and advice about pregnancy risks.
-
Coordination with your healthcare provider if any special issues come up.
-
Help navigating community resources (programs, services) that might benefit you.
-
Answers to your questions about medications or prescriptions during pregnancy.
How It Works
-
The maternity nurse will reach out to you every 3‑6 weeks to check in on how you and your baby are doing.
How to Enroll / Start
-
If you’re newly pregnant, a nurse may contact you about enrolling.
-
To start now, call 1‑800‑641‑3224 and choose option 3.
Who It’s For
If you have one or more of these conditions, this program is designed to support you:
-
Asthma (including pediatric)
-
Chronic kidney disease (CKD)
-
Chronic obstructive pulmonary disease (COPD)
-
Chronic pain
-
Congestive heart failure (CHF)
-
Coronary artery disease (CAD)
-
Diabetes (including pediatric)
-
High blood pressure
What You Get
How to Enroll
-
There is no cost to you.
-
Call 1‑800‑451‑6123 to learn more or to sign up.
Join the Weight Management Program: Positively Me
Managing your weight can be challenging, which is why EMI Health and WebMD Health Services offer tools and support to help. This program is voluntary, confidential, and free. Our mission is to help members build healthy habits through coaching and make lasting progress toward their weight goals.
Learn how to join Positively Me:
- Take the Health Risk Assessment in your BeWell Portal
Your results will include a wellness score and personalized tips to improve your health. - Connect with a health coach
After the assessment, you’ll enter your contact info so a coach can reach out. - A coach will follow-up soon
If you qualify for the program, your coach will contact you directly to help you get started.
Get started today! Download the BeWell app.
- Scan the QR code below to download the Wellness at Your Side app
- Use the connection code: BeWell
- Login with your My EMI Health account credentials
Don’t have an account? Register your My EMI Health account by going to emihealth.com/account.
2026 Formulary List
The EMI Health Prescription Drug Formulary is a helpful tool that shows which medications are covered under your pharmacy plan—and whether they’re listed as generic, preferred brand, or non-preferred brand.
This list helps you:
What to Know
Check Your Plan and Pricing
-
Coverage levels can vary by plan. Be sure to check your Summary of Benefits or Plan Document to see how your plan handles generics, preferred brands, and specialty medications.
-
Use the Pharmacy Tool in your EMI Health member dashboard to compare prices and see what you’ll pay before you fill a prescription.
View or Download the 2026 Prescription Drug Formulary: English | Spanish
SaveonSP Specialty Medications
SaveOnSP Program: What You Should Know
EMI Health offers the SaveOnSP Program in partnership with Express Scripts, Accredo Specialty Pharmacy, and SaveOnSP, LLC. This program helps you pay $0 out‑of‑pocket for certain specialty medications when you enroll and complete the required manufacturer copay assistance process.
-
There's no extra cost to participate.
-
You won’t use up your deductible or reach your out‑of‑pocket maximum for these medications under this program.
-
The program is available to members on both High Deductible and Traditional Plans.
-
If you do not enroll, your copay for qualifying specialty meds will fall under the standard benefit, often about 25% coinsurance.
How to Enroll
To take part in the SaveOnSP Program, you’ll need to: Call 1‑800‑683‑1074 to get started.
Diabetes: Patient Assurance Program (PAP)
Pay no more than $25 for select insulin and diabetes medications
Managing your diabetes shouldn?t come with financial stress. That's why EMI Health, in partnership with Express Scripts, offers a program to lower your out-of-pocket costs on many common insulin and diabetes medications.
If you're enrolled in a participating EMI Health medical plan, you may qualify for capped pricing. Your cost will be $25 or less for a 30-day supply of covered insulin and diabetes medications. The savings apply automatically when you fill your prescription at the pharmacy? no forms or extra steps required. To see the covered medications, click on the flyer below:
Price Assure Guarantee
Price Assure is a built-in program that helps you save money on certain medications—no enrollment needed.
Here’s how it works:
When you fill a prescription at a participating in-network pharmacy, EMI Health automatically checks if the GoodRx discount price is lower than your plan’s cost. If it is, you automatically get the lower price—no coupons, no codes, no hassle.
What You Get
Tip: Always ask your pharmacist to run your EMI Health plan first to get the Price Assure savings, if applicable.

💡
Stay In-Network to Save More on Care
Visiting in-network providers helps you get the most from your EMI Health benefits. In-network doctors, dentists, and specialists have agreed to lower rates—so you’ll usually pay less out of pocket.
Dental
DHMO Provider Selection
This plan requires you to select a participating general dentist who will provide you with all of your care, and refer you to specialists when necessary. You may only change your selection once each month. You may also call our Customer Service Department at (800) 662-5851, Monday through Friday 6:00 a.m.to 6:00 p.m., to inform us of your selection. Your coverage will not be valid until a provider is selected.
Dental Overview - Utah Plans/Networks
Learn how EMI Health dental plans work, including coverage highlights, network access, and how to find in-network providers. Features a QR code for quick access to benefit summaries and provider search tools.
Utah: English
Vision
VSP Overview
VSP is one of the largest and most trusted vision benefits carriers in the U.S., with a network of thousands of eye doctors and optical retailers. EMI Health partners with VSP so you can get dependable vision care wherever you are.
Using your benefit is easy!1. Create an account at vsp.com to see your in-network coverage.2. Check if your plan includes an exam, hardware, or both.3. Find a VSP network doctor or retailer.4. At your visit or purchase, show your EMI Health Member ID card and tell them you have VSP.

ELIGIBILITY
WHO'S ELIGIBLE?
If you are eligible for benefits, you can cover your legal spouse, your children up to age 26, regardless of student or marital status, with the exception of life insurance which would end if your dependent child gets married. Dependents of any age with who are disabled can also be covered.
LIFE EVENT
WHEN YOUR LIFE CHANGES
Due to IRS regulations, you can only elect to make changes to your health insurance coverage during the annual open enrollment unless you experience a qualifying life status change during the year. Qualified events outside the open enrollment period allow you to add and/or remove yourself and your dependents
Common examples of qualifying life status changes are:
- Marriage
- Divorce
- Birth or adoption of a child
- Child reaching age 26 • Death of a spouse or child
- Change in child custody
- Change in coverage elections made by your spouse (or parent) during their employer's open enrollment period
- Loss of coverage under your spouse’s plan
- Loss of coverage under your parent's plan (once you turn age 26)
Documentation of the event, such as a marriage certificate, divorce decree, letter of coverage, or loss of coverage notice is required to finalize the change. If the supporting documentation is not submitted within the allotted timeframe, the earliest opportunity to make changes to your elections would be the next annual open enrollment period. Changes to your health insurance elections due to a qualifying life status change need to be made within 31 days of the event. Notify your HR representative or call EMI Health customer service for help.
COBRA
CONTINUING COVERAGE AFTER TERMINATION
Under most circumstances, you and your dependents may continue to participate in select benefit plans through COBRA after you terminate. You will be advised of your COBRA rights if you experience a COBRA-qualifying event. For more information, contact EMI Health customer service at (800) 662-5851.
COORDINATION OF BENEFITS (COB)
WHAT YOU NEED TO KNOW
If you, your spouse, or any dependents have other health insurance in addition to your EMI Health plan, we’ll need a quick form from you. It’s called a Coordination of Benefits (COB) form, and it helps us understand how your coverage works alongside your other plan.
Why it matters:
Having accurate COB information on file ensures your claims are processed smoothly and prevents delays or overpayments. It also helps us keep your EMI Health plan running efficiently and cost-effectively.
What to do:
Just fill out the COB form and return it to EMI Health as soon as possible.
Need help?
If you’re not sure whether this applies to you or how to complete the form, we’re here to help. Reach out to our Member Services team at (800) 662-5851 (Monday-Friday 6:00 am - 6:00 pm) and we’ll walk you through it.
Download COB Form: English
REAL HELP FROM REAL PEOPLE
Customer Service
Whether you’re looking for help with benefits, claims, ID cards, or something else—we’ve got a knowledgeable, friendly team ready to assist.
Call our Member Services team
(800) 662-5851
Monday - Friday 6:00 am - 6:00 pm
We’re committed to making your experience as smooth as possible. If something doesn’t make sense, just ask—we’ll walk you through it.
.jpg?width=300&height=344&name=customer_service_AdobeStock_219286958%20(1).jpg)
