Affordable Health Basics That Work for You
EMI Health’s MEC (Minimum Essential Coverage) plans cover your preventive care—like checkups, vaccines, and screenings—100% when you stay in-network. You also get perks like $0 TeleMed, Rx discounts, and optional vision/dental savings.
Affordable Health Basics That Work for You
EMI Health’s MEC (Minimum Essential Coverage) plans cover your preventive care—like checkups, vaccines, and screenings—100% when you stay in-network. You also get perks like $0 TeleMed, Rx discounts, and optional vision/dental savings.
Welcome to Your MEC Plan
Your MEC plan gives you essential care and access to a large network of doctors. It’s affordable coverage that supports your everyday health.

Some medicines help keep you healthy and prevent bigger problems later.
If the medicine is on the ACA Preventive Care Drug approved list, your plan covers it at no cost to you as long as you have a prescription from an in-network provider.
View or Download Preventive Care Drug List: English | Spanish

$0 Cost - Available 24/7, even on weekends and holidays
TeleHealth lets you talk to a doctor by phone or video anytime, day or night. You can get help without leaving your home, waiting in a lobby, or paying for an in-person visit.
Doctors can even call in a prescription to your pharmacy when needed.
Included EMI Health Essentials
EMI Health ID Card
You will receive your Member ID Card in the mail after enrollment. The card lists the subscriber's name only, but can be used by all plan members.
Your EMI Health ID card is more than just proof of insurance–it's a quick reference for you and your providers. It lists your plan types, provider networks, and essential contact information.
Each card is personalized based on your coverage. If your card includes medical, dental, and vision plans, each section will appear in its own tab. If you only have one type of coverage (such as dental), all your plan details may appear on one side of the card.
How to Search for a Provider
As a member of EMI Health, you can take advantage of a large choice of in- network providers locally and nationally. To find an in- network provider, follow these steps.
- Go to emihealth.com and click on + FIND A PROVIDER along the upper part of the home page, or use the green button below.
- Choose Search as a Guest*
- Click on either the MEDICAL, DENTAL, or VISION tab, Choose your NETWORK NAME from the drop down menu, Choose your STATE, and click SEARCH.
Scroll down to see a list of participating providers along with their contact information. If you'd prefer to search for a specific provider, enter the PROVIDER NAME in the field and click the SEARCH button.
*If you are already a member, Click Search as a Member, you will be directed to register or login to your My EMI Health Account. From your member dashboard, you can select +Find a Provider and your default networks will be auto-populated. It's a quick and easy way to search for all your in-network providers.
Understanding Claims
Carrier Vs. Network
EMI Health is currently your insurance carrier. We pay your claims, manage your plan, and coordinate your benefits. It's important to remember that we are the main point of contact for eligibility, pre-authorizations, and all other benefit questions. In addition to providing insurance services, we lease provider networks to give you substantial discounts on your medical services and give you the convenience of having in-network provider options wherever you are in the country.
Some of the provider networks we lease are Aetna, Blue Cross Blue Shield, Cigna, or First Health. It will vary depending on what state you are in and your plan. Please check your ID card for your in- state network information and note it may be a different than the out-of- state network.
Your ID card also includes a section for your provider indicating how and where to submit claims. It's important that your claims get submitted to the correct network and that your provider uses the correct claim address (found on your ID card) to ensure you're getting that special rate and the best savings.
EOB's (Explanation of Benefits)
- Log in to your My EMI Health account.
- In the Recent Claims section, to the right of each claim, you will see the View EOB button.
- Filter your results: You can sort your claims by type, family member, time period, or network using the drop down menus at the top. You can see more claims by clicking on Advanced Claims Search.
In less than 30 seconds, you can find the EOB you are looking for. It has never been easier to locate and view your EOBs with EMI Health.
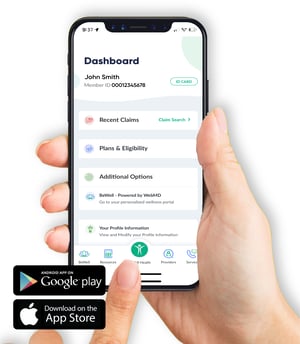
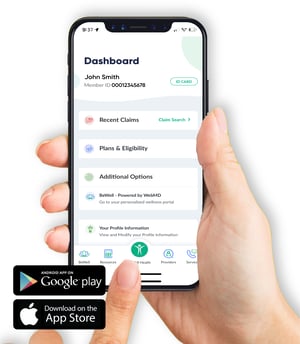
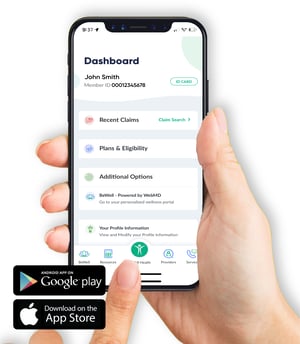
EMI Health Mobile App
Download the EMI Health mobile app to carry your benefits with you wherever you (and your phone) are headed.
Access your BeWell PortalSee your EOBs (Explanation of Benefits)Plan DocumentsSearch for a ProviderView your ID Card
Click to Download the App: For Android | For iPhone
Register your EMI Health Account
 Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Follow these steps:
- Go to https://emihealth.com/Identity/Account/Register
- Choose Member, and click Continue.
- Fill in requested information including your EMI Health Member ID number from your ID card, Click Continue.
My EMI Health Member Dashboard
Your member dashboard gives you a clear view of your benefits—all in one secure place. Use it to track claims, check coverage, download your ID card, and more.
Note: Your dashboard may look different depending on the type of benefits you have.

What You’ll Find on Your Dashboard:
✔ Member ID Card
Quickly view, download, or print your EMI Health member ID card for easy access whenever you need it.
✔ Plan Details
See which plans you're enrolled in and get quick links to plan documents like benefit summaries and coverage guides.
✔ Accumulators
Get real-time updates on how much you’ve paid toward your deductible and out-of-pocket maximum for medical and dental plans.
✔ Claims & EOBs
Check the status of your recent claims and view Explanation of Benefits (EOB) statements to understand what’s been paid and what you might owe.
✔ Provider Search
Use our upgraded search tool to find in-network doctors, dentists, and specialists—now with filters to help you narrow your results.
✔ Resource Library
Browse helpful forms, articles, and answers to common questions—all in one convenient place.
BenefitHub Discounts
Enjoy deals and discounts at your favorite stores and on your favorite brands just because you're a member of EMI Health. Discounts on over 100,000 name brands at hundreds of your favorite retailers. Find tickets to sporting events, concerts, theaters, movies and theme parks. Shop restaurants, gyms, Groupon deals and thousands of other local offers.
Start saving now:
1. Go to https://emi.benefithub.com/Welcome2. Click Create Account.3. Enter Referral Code: NV6ADR4. Enter your email address5. Click Create Account.
View or Download Flyer: English

Tips to Save on RX:
Refill maintenance medications through home deliveryReach out to Express Scripts Member Services at 866-815-0003 for support anytime.
Your MEC Plus Plan
Your EMI Health MEC Plus Plan is designed to give you affordable access to the care and support you use most—so you can take care of your health without the high cost of traditional insurance

Medications from the ACA list are covered at 100%.
For other needs, generic drugs are covered at 50%, so you pay half the cost. You can fill your prescriptions at many pharmacies, including Walgreens.
If you take a medicine every day, you can also use Express Scripts mail order to get a 90-day supply, which can save you time and money.
View or Download Preventive Care Drug List: English | Spanish
View or Download 2025 MEC Generic Drug List: English | Spanish

$0 Cost - Available 24/7, even on weekends and holidays
TeleHealth lets you talk to a doctor by phone or video anytime, day or night. You can get help without leaving your home, waiting in a lobby, or paying for an in-person visit.
Doctors can even call in a prescription to your pharmacy when needed.
Included EMI Health Essentials
EMI Health ID Card
You will receive your Member ID Card in the mail after enrollment. The card lists the subscriber's name only, but can be used by all plan members.
Your EMI Health ID card is more than just proof of insurance–it's a quick reference for you and your providers. It lists your plan types, provider networks, and essential contact information.
Each card is personalized based on your coverage. If your card includes medical, dental, and vision plans, each section will appear in its own tab. If you only have one type of coverage (such as dental), all your plan details may appear on one side of the card.
How to Search for a Provider
As a member of EMI Health, you can take advantage of a large choice of in- network providers locally and nationally. To find an in- network provider, follow these steps.
- Go to emihealth.com and click on + FIND A PROVIDER along the upper part of the home page, or use the green button below.
- Choose Search as a Guest*
- Click on either the MEDICAL, DENTAL, or VISION tab, Choose your NETWORK NAME from the drop down menu, Choose your STATE, and click SEARCH.
Scroll down to see a list of participating providers along with their contact information. If you'd prefer to search for a specific provider, enter the PROVIDER NAME in the field and click the SEARCH button.
*If you are already a member, Click Search as a Member, you will be directed to register or login to your My EMI Health Account. From your member dashboard, you can select +Find a Provider and your default networks will be auto-populated. It's a quick and easy way to search for all your in-network providers.
Understanding Claims
Carrier Vs. Network
EMI Health is currently your insurance carrier. We pay your claims, manage your plan, and coordinate your benefits. It's important to remember that we are the main point of contact for eligibility, pre-authorizations, and all other benefit questions. In addition to providing insurance services, we lease provider networks to give you substantial discounts on your medical services and give you the convenience of having in-network provider options wherever you are in the country.
Some of the provider networks we lease are Aetna, Blue Cross Blue Shield, Cigna, or First Health. It will vary depending on what state you are in and your plan. Please check your ID card for your in- state network information and note it may be a different than the out-of- state network.
Your ID card also includes a section for your provider indicating how and where to submit claims. It's important that your claims get submitted to the correct network and that your provider uses the correct claim address (found on your ID card) to ensure you're getting that special rate and the best savings.
EOB's (Explanation of Benefits)
- Log in to your My EMI Health account.
- In the Recent Claims section, to the right of each claim, you will see the View EOB button.
- Filter your results: You can sort your claims by type, family member, time period, or network using the drop down menus at the top. You can see more claims by clicking on Advanced Claims Search.
In less than 30 seconds, you can find the EOB you are looking for. It has never been easier to locate and view your EOBs with EMI Health.
EMI Health Mobile App
Download the EMI Health mobile app to carry your benefits with you wherever you (and your phone) are headed.
Access your BeWell PortalSee your EOBs (Explanation of Benefits)Plan DocumentsSearch for a ProviderView your ID Card
Click to Download the App: For Android | For iPhone
Register your EMI Health Account
 Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Follow these steps:
- Go to https://emihealth.com/Identity/Account/Register
- Choose Member, and click Continue.
- Fill in requested information including your EMI Health Member ID number from your ID card, Click Continue.
My EMI Health Member Dashboard
Your member dashboard gives you a clear view of your benefits—all in one secure place. Use it to track claims, check coverage, download your ID card, and more.
Note: Your dashboard may look different depending on the type of benefits you have.

What You’ll Find on Your Dashboard:
✔ Member ID Card
Quickly view, download, or print your EMI Health member ID card for easy access whenever you need it.
✔ Plan Details
See which plans you're enrolled in and get quick links to plan documents like benefit summaries and coverage guides.
✔ Accumulators
Get real-time updates on how much you’ve paid toward your deductible and out-of-pocket maximum for medical and dental plans.
✔ Claims & EOBs
Check the status of your recent claims and view Explanation of Benefits (EOB) statements to understand what’s been paid and what you might owe.
✔ Provider Search
Use our upgraded search tool to find in-network doctors, dentists, and specialists—now with filters to help you narrow your results.
✔ Resource Library
Browse helpful forms, articles, and answers to common questions—all in one convenient place.
BenefitHub Discounts
Enjoy deals and discounts at your favorite stores and on your favorite brands just because you're a member of EMI Health. Discounts on over 100,000 name brands at hundreds of your favorite retailers. Find tickets to sporting events, concerts, theaters, movies and theme parks. Shop restaurants, gyms, Groupon deals and thousands of other local offers.
Start saving now:
1. Go to https://emi.benefithub.com/Welcome2. Click Create Account.3. Enter Referral Code: NV6ADR4. Enter your email address5. Click Create Account.
View or Download Flyer: English

Tips to Save on RX:
Refill maintenance medications through home deliveryReach out to Express Scripts Member Services at 866-815-0003 for support anytime.
Your MEC Enhanced Plan
Your MEC Enhanced plan builds on preventive care by adding low-cost doctor visits, urgent care, stronger prescription coverage, and discounts for dental and vision. It’s the best option if you want more protection and more ways to get care.

MEC Enhanced covers your preventive care at 100%, like checkups and screenings.
You also get:
-
3 primary care visits per year
-
3 specialist visits per year
-
3 convenience clinic visits per year
-
3 urgent care visits per year
Additional covered services:
-
3 minor diagnostic visits per year (labs, x-rays)
-
1 MRI/CT scan per year
-
1 in-office surgery per year (covered at 100%)
-
3 injections or anesthesia services per year (covered at 100%)
Each visit has a low copay where applicable.
Always check your Plan Summary for copay amounts and full details.

MEC Enhanced also helps you save on many other medicines:
-
Generic drugs: You pay 10% of the cost
-
Preferred brand drugs: You pay 50% of the cost
You can fill your prescriptions at many pharmacies, including Walgreens.
If you take a medicine every day, you can also use Express Scripts mail order to get a 90-day supply, which can save you time and money.
Check your Plan Summary for all cost-share amounts and full details.
View or Download Preventive Care Drug List: English | Spanish
View or Download 2025 MEC Generic Drug List: English | Spanish

$0 Cost - Available 24/7, even on weekends and holidays
TeleHealth lets you talk to a doctor by phone or video anytime, day or night. You can get help without leaving your home, waiting in a lobby, or paying for an in-person visit.
Doctors can even call in a prescription to your pharmacy when needed.
Included EMI Health Essentials
EMI Health ID Card
You will receive your Member ID Card in the mail after enrollment. The card lists the subscriber's name only, but can be used by all plan members.
Your EMI Health ID card is more than just proof of insurance–it's a quick reference for you and your providers. It lists your plan types, provider networks, and essential contact information.
Each card is personalized based on your coverage. If your card includes medical, dental, and vision plans, each section will appear in its own tab. If you only have one type of coverage (such as dental), all your plan details may appear on one side of the card.
How to Search for a Provider
As a member of EMI Health, you can take advantage of a large choice of in- network providers locally and nationally. To find an in- network provider, follow these steps.
- Go to emihealth.com and click on + FIND A PROVIDER along the upper part of the home page, or use the green button below.
- Choose Search as a Guest*
- Click on either the MEDICAL, DENTAL, or VISION tab, Choose your NETWORK NAME from the drop down menu, Choose your STATE, and click SEARCH.
Scroll down to see a list of participating providers along with their contact information. If you'd prefer to search for a specific provider, enter the PROVIDER NAME in the field and click the SEARCH button.
*If you are already a member, Click Search as a Member, you will be directed to register or login to your My EMI Health Account. From your member dashboard, you can select +Find a Provider and your default networks will be auto-populated. It's a quick and easy way to search for all your in-network providers.
Understanding Claims
Carrier Vs. Network
EMI Health is currently your insurance carrier. We pay your claims, manage your plan, and coordinate your benefits. It's important to remember that we are the main point of contact for eligibility, pre-authorizations, and all other benefit questions. In addition to providing insurance services, we lease provider networks to give you substantial discounts on your medical services and give you the convenience of having in-network provider options wherever you are in the country.
Some of the provider networks we lease are Aetna, Blue Cross Blue Shield, Cigna, or First Health. It will vary depending on what state you are in and your plan. Please check your ID card for your in- state network information and note it may be a different than the out-of- state network.
Your ID card also includes a section for your provider indicating how and where to submit claims. It's important that your claims get submitted to the correct network and that your provider uses the correct claim address (found on your ID card) to ensure you're getting that special rate and the best savings.
EOB's (Explanation of Benefits)
- Log in to your My EMI Health account.
- In the Recent Claims section, to the right of each claim, you will see the View EOB button.
- Filter your results: You can sort your claims by type, family member, time period, or network using the drop down menus at the top. You can see more claims by clicking on Advanced Claims Search.
In less than 30 seconds, you can find the EOB you are looking for. It has never been easier to locate and view your EOBs with EMI Health.
EMI Health Mobile App
Download the EMI Health mobile app to carry your benefits with you wherever you (and your phone) are headed.
Access your BeWell PortalSee your EOBs (Explanation of Benefits)Plan DocumentsSearch for a ProviderView your ID Card
Click to Download the App: For Android | For iPhone
Register your EMI Health Account
 Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Once you receive your Member ID card and/or have your Member ID number, you can go online and create your account. From your member dashboard you'll find everything you need to utilize your EMI Health benefits. Please note that you will only make an account for your family through your plan subscriber. Dependents and spouses will not have their own account.
Follow these steps:
- Go to https://emihealth.com/Identity/Account/Register
- Choose Member, and click Continue.
- Fill in requested information including your EMI Health Member ID number from your ID card, Click Continue.
My EMI Health Member Dashboard
Your member dashboard gives you a clear view of your benefits—all in one secure place. Use it to track claims, check coverage, download your ID card, and more.
Note: Your dashboard may look different depending on the type of benefits you have.

What You’ll Find on Your Dashboard:
✔ Member ID Card
Quickly view, download, or print your EMI Health member ID card for easy access whenever you need it.
✔ Plan Details
See which plans you're enrolled in and get quick links to plan documents like benefit summaries and coverage guides.
✔ Accumulators
Get real-time updates on how much you’ve paid toward your deductible and out-of-pocket maximum for medical and dental plans.
✔ Claims & EOBs
Check the status of your recent claims and view Explanation of Benefits (EOB) statements to understand what’s been paid and what you might owe.
✔ Provider Search
Use our upgraded search tool to find in-network doctors, dentists, and specialists—now with filters to help you narrow your results.
✔ Resource Library
Browse helpful forms, articles, and answers to common questions—all in one convenient place.
BenefitHub Discounts
Enjoy deals and discounts at your favorite stores and on your favorite brands just because you're a member of EMI Health. Discounts on over 100,000 name brands at hundreds of your favorite retailers. Find tickets to sporting events, concerts, theaters, movies and theme parks. Shop restaurants, gyms, Groupon deals and thousands of other local offers.
Start saving now:
1. Go to https://emi.benefithub.com/Welcome2. Click Create Account.3. Enter Referral Code: NV6ADR4. Enter your email address5. Click Create Account.
View or Download Flyer: English
MEC Enhanced Dental Discount Plan
If you have the MEC Enhanced Plan, you also get access to discounted dental services through EMI Health’s Value Dental Plan. This is not insurance—it’s a discount program that helps you save on most dental procedures when you visit participating in-network providers.
It's easy to use:
- Show your EMI Health ID Card at a participating dental provider.
- Pay the discounted rate directly to the dentist at the time of service.
There are NO deductibles, NO annual maximums, and NO waiting periods.

| Procedure | Typical Member Cost Range |
| Routine Oral Exam | $15–$25 |
| Adult Teeth Cleaning | $35–$55 |
| X-Rays (Bitewing, set of 4) |
$20–$35 |
| Child Fluoride Treatment | $15–$25 |
| Filling (1 surface, composite) | $60–$90 |
| Simple Tooth Extraction | $60–$100 |
| Contact Lens Exam (fit & evaluation) | 15% off |
Vision Discount with VSP Choice

You and your family automatically get access to discounted vision services through the VSP Choice Network—included with all MEC plans.
What You Get with VSP Discount Vision:
| Service | Your Cost/Savings |
| WellVision Eye Exam | $50 with glasses purchase, 20% off without |
| Retinal Screening | Guaranteed pricing with exam - max $39 |
| Lenses (with glasses purchase) |
Single Vision $40, Lined Bifocals $60, Lined Trifocals $75 |
| Polycarbonate Lenses (Children) | $0 |
| Lens Enhancements | Save 20–25% on scratch-resistant, progressive, or anti-glare coatings |
| Frames | 25% off when buying a complete pair of glasses |
| Contact Lens Exam (fit & evaluation) | 15% off |
First Health Limited Benefit Network
-
Arizona, Georgia & Texas
EMI Health MEC plans use the same network both in-state and when traveling out of state—making it easy to get care wherever you go. The only exception is Utah, where EMI Health uses its own MEC Network.
1. What It Is
-
A national PPO network operated by First Health (an Aetna/CVS Health company), featuring access to over 6,400 hospitals, 151,000 ancillary facilities, and 1.2 million healthcare professionals.
-
It’s classified as a Limited Benefit Plan network, built to deliver affordable care at discounted rates for preventive and in‑network services.
2. Why It Matters for MEC
-
Guaranteed access to preventive care at 100% coverage, when you use in‑network providers.
-
Deep discounts (typically 32–52% off) on non-covered services like urgent care, lab tests, x-rays, and more.*
3. How It Works
-
In-Network: When you receive care from a network provider, you automatically get discounted rates—your provider will file the claim.
-
Out-of-Network: Services aren’t discounted or covered, and you’re responsible for the full cost.
4. Special Notes
-
Preventive services are only 100% covered in-network.
-
Some elective diagnostic tests (like MRIs/labs) must be performed at free-standing facilities, not hospital-based, to stay in-network—avoid surprise costs.*
-
Always confirm provider participation before receiving services to avoid unexpected costs
*Always check your plan summary to see what services are covered. Coverage varies depending on MEC plan. Only the MEC Enhanced plan has coverage for some diagnostic services.
Need help finding a provider or questions about coverage in your area? Call Customer Service, 1-800-662-5851, Monday-Friday, 6:00 am - 6:00 pm, MST.

“Can I go to a free-standing facility in the First Health network?”
.jpg?width=400&height=459&name=customer_service_AdobeStock_219286958%20(1).jpg)
Customer Service
Whether you’re looking for help with benefits, claims, ID cards, or something else—we’ve got a knowledgeable, friendly team ready to assist.
We’re committed to making your experience as smooth as possible. If something doesn’t make sense, just ask—we’ll walk you through it.


