Prescription Drugs (RX)
SmithRx partners with over 83,000 retail pharmacies across the nation including the major national chains, regional chains, grocers and independent pharmacies. In addition, we have three preferred mail order pharmacies and two specialty pharmacies. You can always find the pharmacy with the best price by using the Find My Meds search tool in the Member Portal at mysmithrx.com.
Medication Tiers & Common Cost Patterns
| Tier | Retail (30-day supply) | Home Delivery (90-day supply) |
| Generic Drugs | Lowest Cost | Usually 2x Retail |
| Preferred Brands | Mid-range Cost | Savings with 90-day fill |
| Non-Preferred | Highest Cost | Better Value by mail order |
Traditional Copay Plan Members
- You may have a separate prescription deductible, or you may pay copays by drug tier from day one.
(Q)HDHP Plan Members
- You’ll pay the full cost of prescriptions until your combined medical and pharmacy deductible is met. After that, your plan starts sharing the cost.
For your exact pricing and benefit details, check your plan summary (found in your enrollment booklet or online member portal).
Ways to Fill Prescriptions
Retail Pharmacies
Over 83,000 in-network locations for short-term needs
Including:


![]()
![]()
![]()
Home Delivery
Great for ongoing medications; usually saves time and money
![]()



FAQ
Commonly asked questions about SmithRX pharmacy benefits.
What if a member wants to check the price of their medication at various pharmacies?
Members can access the Find My Meds pricing tool by registering for the SmithRx member portal at www.mysmithrx.com.
Within the tool, they can enter various drug details (ex: name, strength, quantity, and day supply) and find the price of the drug at pharmacies within a selected zip code or city.
What if a member gets a rejection at the pharmacy?
Members should follow these steps:
1. Make sure they have brought their new or most updated ID card to the pharmacy.
2. Make sure the pharmacy is using the correct/updated insurance information.
3. Ask the pharmacy to explain the rejection.
4. If the member or pharmacy still has questions, call SmithRx at 844-454-5201 immediately, ideally while the member is still at the pharmacy.
What if a drug has a prior authorization (PA) requirement?
Members can identify PA drugs using the formulary lookup tool on the member portal.
Members should advise their doctor to fax completed PA forms to SmithRx. 866-642-5620
Prescribers should call SmithRx with any questions. 844-512-3030
If members have questions about the PA, they should reach out to the SmithRx member support team. Online chat at www.smithrx.com, email help@smithrx.com, or call 844-454-5201.
What if a drug has a step therapy (ST) requirement and the member wants to understand the process?
Members can identify ST drugs using the formulary lookup tool on the member portal. Members should reach out to the SmithRx member support team. Online chat at www.smithrx.com, email help@smithrx.com, or call 844-454-5201.
What if a member wants to check the price of their medication at various pharmacies?
Members can access the Find My Meds pricing tool by registering for the SmithRx member portal at www.mysmithrx.com.
Within the tool, they can enter various drug details (ex: name, strength, quantity, and day supply) and find the price of the drug at pharmacies within a selected zip code or city.
What if a member’s drug is considered specialty?
Members can identify specialty drugs using the Formulary Lookup tool on the member portal. Members should advise their doctor to send the script to Kroger Specialty or Senderra Rx.
- Kroger Specialty Pharmacy: Patients can reach Kroger Specialty Pharmacy for enrollment assistance by calling 888-355-4191. Prescribers can visit www.krogerspecialtypharmacy.com and fill out the appropriate forms for the appropriate department.
- Senderra Rx: Patients can reach Senderra for enrollment assistance by calling 888-777-5547. Prescribers can visit https://senderrarx.com/prescribers and fill out the appropriate forms for the appropriate department.
Once the member’s prescriber has sent the script to the specialty pharmacy, the member should call the pharmacy to provide their insurance information and to schedule delivery.
What if a member wants to use mail order?
Members can utilize our mail order partner pharmacies for convenience and savings. Our standard mail order partner is Amazon, but some members might end up using Walmart Home Delivery if they are on particular drugs, and that would be communicated to them by our Connect team.
Amazon Pharmacy: Patients can register at www.amazon.com/smithrx and reach the pharmacy at 855-745-5725.
Prescribers can send prescriptions via electronic prescribing, fax or phone:
● Name/E-scribe: Amazon Pharmacy Home Delivery● Amazon Pharmacy fax: 512-884-5981● Amazon prescriber and pharmacy line: 855-206-3605 smithrx.com Pharmacy Benefits FAQ for Members
Walmart Home Delivery: Patients can reach out for enrollment assistance by calling 800-273-3455, by email at wmsrx@wal-mart.com, or register at https://www.walmart.com/cp/pharmacy-mail-order/1042239.
Prescribers can send prescriptions via electronic prescribing, fax or phone:
● Walmart Pharmacy fax: 800 406-8976● Walmart prescriber and pharmacy line: 800 273-3455● Website: https://www.walmart.com/cp/1042239
Mark Cuban's Cost Plus (MCCP) pharmacy is another in-network mail order option. Members can check the Cost Plus website to see if generic medications are available there for a lower cost than what they are paying at retail. Additionally, the SmithRx Connect team may reach out to members about transitioning certain medications to MCCP.
Mark Cuban Cost Plus Drugs: Patients can see whether their medications are available at https://costplusdrugs.com/medications, contact the pharmacy by completing the form at costplusdrugs.com/contact/support, or contact Truepill (NPI: 1851947139) at (650) 353-5495.
Once your script has been sent by your prescriber to Mark Cuban Cost Plus Drug Company, you can register at costplusdrugs.com.
Prescribers can send prescriptions via electronic prescribing to:
● Name/E-scribe: Mark Cuban Cost Plus Drug Company (MCCPD)
What if a member is looking for more information on the cost, shipment, or delivery of their mail order or specialty medication?
Members should reach out directly to the pharmacy that processed their medication.
What if a member receives an email, call, or text from SmithRx?
Members should respond as soon as possible to the email or the phone number from the voicemail or text they received. Members can also reach out via online chat at www.smithrx.com, email help@smithrx.com, or call 844-454-5201.
SmithRX Pharmacies
SmithRx partners with over 83,000 retail pharmacies across the nation including the major national chains, regional
chains, grocers and independent pharmacies. In addition, we have three preferred mail order pharmacies and two specialty pharmacies.
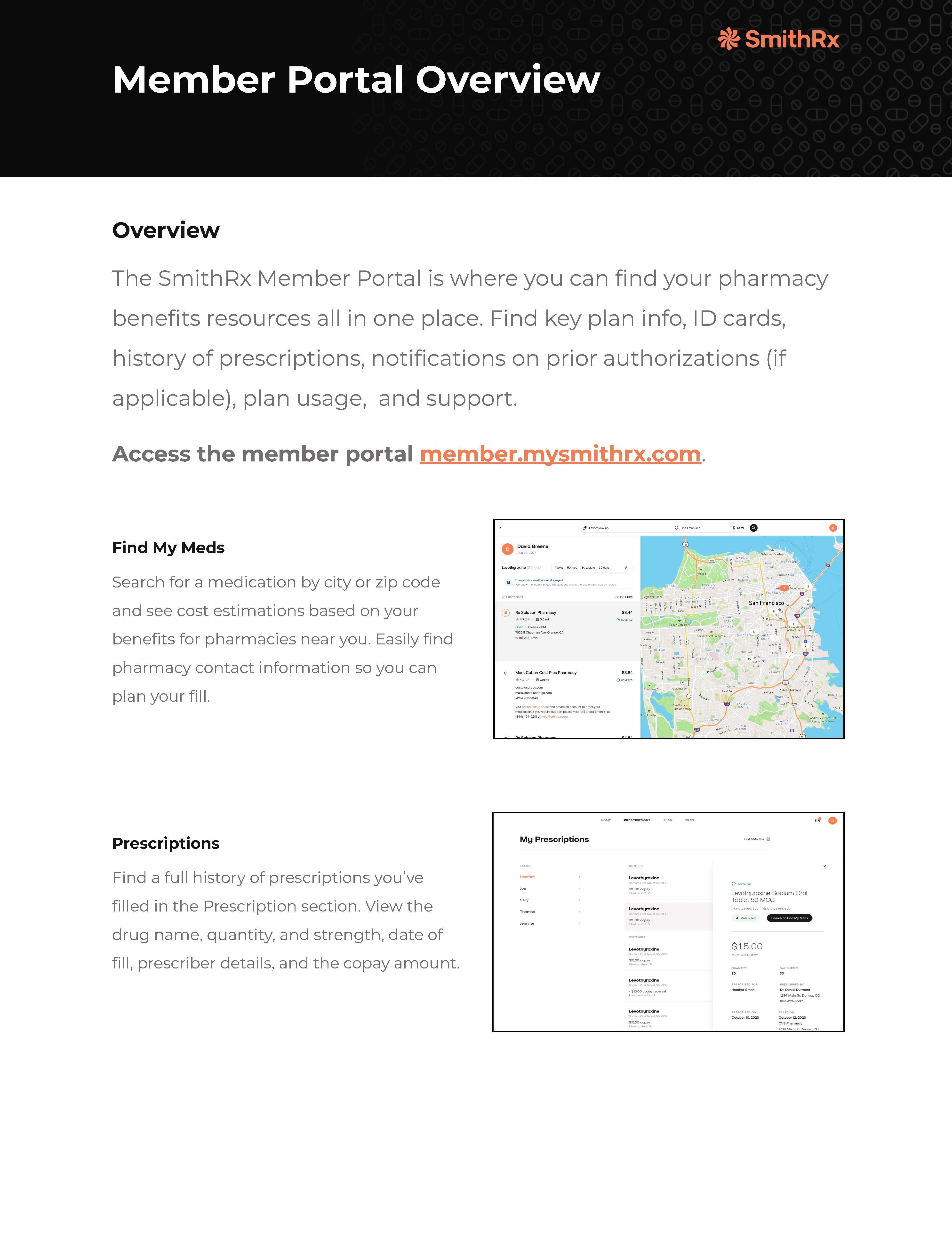
Member Portal Overview
The SmithRx Member Portal is where you can find your pharmacy benefits resources all in one place. Find key plan info, ID cards, history of prescriptions, notifications on prior authorizations (if applicable), plan usage, and support.
.jpg?width=400&height=459&name=customer_service_AdobeStock_219286958%20(1).jpg)
Customer Service
Whether you’re looking for help with benefits, claims, ID cards, or something else—we’ve got a knowledgeable, friendly team ready to assist.
We’re committed to making your experience as smooth as possible. If something doesn’t make sense, just ask—we’ll walk you through it.